|
Posts by: Tori Houle, Lifestyle Contributor and Junior Editor of PetHealthNetwork Just because the temperature is dropping, doesn't mean your dog wants to play inside now. One of Harley's favorite things do as the weather changes in play in the giant piles of leaves that fill up our yard. However, it's extremely important to be aware that tick season is not over. While you mostly find ticks in tall grass, they also lurk about in the leaves your dog loves to play in. So here's a simple reminder to always be checking your pets, as well as yourself for ticks year round! Ticks are terrible little parasites that carry multiple, nasty diseases that can affect both animals and people. Ticks are almost so common, people sometimes dismiss them as a concern, but it’s so important for pet parents to take ticks seriously. To protect your dog from tick-borne disease, it’s important you know where to be checking for ticks, and how often.
Ticks are still here While the weather is changing and our summer activities are winding down, that doesn’t mean ticks are going into hibernation. Some disease-carrying ticks have actually become immune to the cold because they’ve developed a type of anti-freeze glycoprotein to survive in harsh conditions. How scary is that? Read more about ticks and cold weather here >> Where should you be checking for ticks, and how often? When my dog Harley was diagnosed with Lyme disease 2 years ago, I knew I had to step my game up when it came to checking her for ticks. As demonstrated in the video above, Dr. Paul says that important places to check your dog include:
When should you be using tick preventives? The simple answer to this is always. Ticks are prevalent year-round. If you’re unsure about disease in your environment, check this map to see which canine vector-borne diseases are in your area >>Want more information on ticks? Here are some great resources: Ticks 101 >> Dogs, Ticks and Tick-Borne Parasites >> Protecting Your Dog from Fleas and Ticks >> 6 Tick-Borne Diseases You Should Know About >> If you have any questions or concerns, you should always visit or call your veterinarian -- they are your best resource to ensure the health and well-being of your pets. Reviewed by: Dr. Alexis Seguin, DVM, MS, DACVIM
0 Comments
Post by: Jason Carr, Former Pet Health Network Editor-in-Chief If you’ve ever spent time online you know that most people just can’t get enough of those bizarre cat quirks. Some feline habits are adorable and endearing, while others are confusing and even dangerous. If you’ve ever wondered about certain, strange cat behaviors, you’ve come to the right place to learn. Why Cats StareSo why is my cat staring at me? Most likely, your cat is checking you out and stalking you. While I don’t want to anthropomorphize what’s really going on in your cat’s head while she stares at you, I often feel it’s due to the predator’s instinct. Chalk this up with your cat’s curious nature. Your cat is staring as she literally checks you over. Personally, I believe cats are trying to mind control us into feeding them. "I’m staring at you so you feel guilty and feed me more." Don’t fall for it – give them some entertainment and environment enrichment instead, and let them take out their predator’s stare on a Buster® Cube or Roll-a-Treat ball instead. Medical causes of staring Rarely, medical causes can result in the staring appearance. Several leading causes of death in cats may be associated, including chronic medical problems such as: If untreated, severe hypertension (e.g., high blood pressure) can result. Normal systolic blood pressure for a cat should be approximately 120 mm Hg (similar to humans); if it climbs over 180-200 mm Hg, ocular injury can occur. With high blood pressure, the retina (the “film” of the back of the eye that causes the appearance of “red eye” can detach [called a retinal detachment], causing a dilated pupil. It may look like your cat is staring. If you notice constantly dilated pupils and staring, get to a veterinarian for a blood pressure check. Otherwise, chalk it up to your cat’s predatory drive and attempt to guilt you into something… Why Cats Sleep So MuchRecently, I was watching my own cats as they slept and thought to myself “I wish I could sleep like a cat!” I love to sleep and nap. I bet you do too. (Do you remember when getting you to bed was a battle royale with your parents?) Domestic cats can rarely be accused of overexerting themselves. Cats seem genetically programmed to sleep. In fact, cats can sleep as much as 16 hrs a day and older cats may sleep 18-20 hrs a day1! Why all this sleep? Sleeping helps cats conserve energy, but they probably are not “sleeping” as much as you think. Sleeping, snoozing or “resting their eyes” — while all of these forms of sleeping may look alike, about 75% of a cat’s sleeping time is in “light sleep.” They are easily awakened when they need to be (for example, to protect themselves or to take advantage of a meal). You can recognize when cats are in light sleep because their ears twitch and respond to sound even if their eyes do not open. Cats are capable of sleeping when they are in a sitting position. (That’s not so special!) Cats do sleep deeply sometimes. About 25% of their sleeping time is spent in very deep sleep. Some older cats may sleep deeply as much as 40% of the time. (Sound good to you?) Cats also have a unique sleep/wake cycle. Learn more about it here. Sleeping behavior One of the things I still enjoy most is watching my cats as they dream. They seem to run in their sleep at times and often chatter and vocalize— they may be chasing an imaginary butterfly or lizard. It is common for cats to snore when sleeping. My own cat will often cover his eyes and in a few minutes he is sawing proverbial logs. All of these sleep associated behaviors of cats are normal to one degree or other. It is important as with other behaviors to be familiar with what is normal for your cat. Changes in sleep habits can be associated with a variety of factors, but should be observed and evaluated by your veterinarian as part of your cat's annual physical evaluation. Why Cats Chew Electrical CordsA dangerous household item cats often chew is electrical cord and wire. As with plastic bags, cats can find the oral sensation of chewing on cords pleasant. Kittens in particular can chew cords as part of their exploratory development. Chewing on cords is a dangerous activity that should be actively prevented as it presents a choking hazard, as well as the possibility of injury and death from electrocution. It also can obviously damage your household electronics and cause electrical fires. What’s so great about chewing cords? One reason that cats will chew cords can be related to their dental health, and if you find your cat engaging in these activities, a trip to the veterinarian to make sure her teeth are in good order is important. You may also want to discuss with your veterinarian your cat’s diet, as chewing on odd objects can be a symptom of insufficiency in daily dietary needs. Finally, boredom can be a major factor in habits like these. You should adopt a plan combining management (to keep your cat safe) and enrichment (to engage physical and mental needs). Tips to keep your cat from chewing cords.
Why Cats "Talk"Talking to our cats is often a normal part of our relationship with them. We chat away while not really expecting that they understand our complex sentences or even some of our succinct commands. Yet when they ‘talk’ to us, we are often frustrated by our inability to interpret their meaning or intention. This is especially true with our feline friends. Why is your cat talking to you? Is she upset or not? What does she want or need? Cats do talk Firstly, your cat may be perfectly fine. This is most often the case. Individual cats have their own unique personalities. Some are chatty and some are not. There are even certain breeds (like Siamese cats) that tend, by nature, to be more vocal. Certainly there are times when it’s absolutely normal for a cat to be more vocal (like when there are other strange cats in the vicinity or during breeding season) — especially if your cat has not been spayed or neutered. You know your cat better than anyone. That makes you the best authority on what is normal and also puts you in the best position to notice any increase in your cat’s vocalization patterns or habits. If your cat is talking more, what are the possible reasons for that change? Could my talking cat be trying to tell me something is wrong? Pain or discomfort can certainly make your cat cry out – whether it’s due to hunger or thirst, injury or arthritis, or even weakness. Your cat may be crying or talking more in order to put a voice to her physical distress. If you think your cat’s vocalizations may indicate a physical problem, consult your veterinarian to explore those possibilities. My cat’s a senior. Could she be “senile?” As is the case with humans, altered perception can result in increased vocalization. This tends to be especially true of older cats and often times is more apparent (or just more bothersome) at night. Just like us, as our cats age, they can experience diminished vision or hearing and may even develop cognitive dysfunction or senility. There are medications that may help with confusion and senility. If your cat cannot see, hear or even smell or simply becomes confused by her surroundings, she may cry out. Some owners might not immediately recognize impending hearing or vision loss in a cat; fortunately, routine testing could reveal these types of problems and some causes of diminished sight can be treated (like cataracts). Absolutely mention these concerns when you take your cat in for her checkups. You might also consider keeping your cat closer to you at night, leaving nightlights on and maybe even playing music. What other medical conditions would cause cats to talk more? Other physiological disorders that can cause increased crying and meowing in cats include:
Why Cats Chew Plastic BagsQuestions that can come up when working with families that have cats in their households, are often about a cat’s predilection for chewing on odd items. While plastic bags may seem like a strange choice for cats; from a cat’s point of view, they are very attractive. However, chewing on these bags can be dangerous for your cat as they can suffocate or choke on bags and bag pieces. What’s so great about chewing plastic bags? Plastic bags that come from a grocery or other food store can carry the lingering scent and even taste of food, which makes chewing them a pleasant experience. Many bags are also coated in substances such as cornstarch, stearates (salts of stearate acid), or are made of animal by-products such as gelatin, which makes them attractive to cats. Cats can also enjoy the crinkly noises that a plastic bag makes. Another reason that cats will chew bags can be related to their dental health. If you find your cat engaging in these activities, a trip to the veterinarian to make sure her teeth are in good order is important. You may also want to discuss with your veterinarian your cat’s diet, as chewing on odd objects can be a symptom of insufficiency in daily dietary needs. Finally, boredom can be a major factor in habits like these. You should adopt a plan combining management (to keep your cat safe) and enrichment (to engage your cat’s physical and mental needs). Tips to keep your cat from chewing plastic bags.
Why Cats Run From the Litter BoxBoy, we cat lovers love our cats! Sometimes, to the point of an obsession! We watch their every move and want to understand just what they are doing and why. One of the things cat guardians seem perhaps overly curious about is why cats, after a bowel movement, sometimes leap from their litter box and dart away as if they are being chased. I have observed my own cat running from the litter box so quickly that he hadn’t quite finished “his business.”
Internet speculation: why do cats poop and run? I’ve recently come across an article by Amanda Bernocco, on HNGN, that speculates on this very issue. The posting says that “expert speculation” has finally revealed “a very scientific reason” why some cats might bolt out of their litter boxes after defecation (very exciting indeed). Bernocco goes on to say that cats are running because, in the wild, the smell of poop will attract predators. Unfortunately, while the blog does name an “experienced pet writer (Lori Soard),” it’s unclear how the information was scientifically tested. No specific experts in veterinary medicine or animal behavior are mentioned, nor does it provide any references to scientific research on the matter. Therefore, while I find the speculation very interesting, I’d need to see more support before agreeing with this article's conclusion. Medical reasons for a cat to poop and run Bernocco’s article touches on the fact that some cats may run from their litter box after eliminating either urine or feces if they experience discomfort from the process. This important point I can confirm, and want to give special attention. Such discomfort could be caused by infections or inflammatory processes involving the urinary tract, colon or rectum. It could even be caused by constipation issues. However, once such medical conditions are ruled out (and they most certainly should be), any other ‘psychological’ reason for running away, after eliminating, seems not yet to be science, but rather pure conjecture (which can still be fun). Click here for more about the diagnostic value of the litter box. What do the experts say? Consider how extremely variable the behavior of covering up feces is in the cat world. Some cats do and some cats don’t, even in the wild. According to Feline Behavior Guidelines from the American Association of Feline Practitioners’, “The cat may or may not turn to sniff or cover eliminations.” Newmanveterniary.com says, “Some cats cover feces and urine...some do not.” Dr. Ilona Rodan, a veterinarian and feline specialty behavior consultant, is quoted in an animalplanet.com article as saying that, “she hadn't found evidence that cats run from their waste in the wild.” The same article touches on several additional theories for this behavior, put forward by both Rodon and Carole Wilbourn (cat therapist), including:
It’s understandable that we should all want, almost desperately, to understand what is going on inside the hearts and minds of our feline friends. Do they do what they do because they are happy, sad, anxious or excited? It would be nice to know, but for now I will just have to accept that the exact reason my cat flies out of the litter box, like a booster rocket, will just be one of many mysteries of innate cat-ness. I have found the best explanation to be “There he goes again!” Isn’t it exciting that there are still so many things to learn about these magical and mysterious animals? Post by: Dr. Phil Zeltzman, DVM, DACVS, CVJ Dr. Phil Zeltzman is a mobile, board-certified surgeon in Allentown, PA. Find him online at www.DrPhilZeltzman.com. He is the co-author of “Walk a Hound, Lose a Pound” (www.WalkaHound.com). Common questions I hear from clients include "Is he too old for this surgery?" and "Do you think it's worth it to her because of her age?" Invariably, and with a smile, my answer is "Age is not a disease." This answer is more serious than it sounds (My "mature" clients actually love that quote!). Cancer, kidney malfunction, a hormone imbalance -- those are diseases, which can be treated. But age in and of itself is not a disease. Granted, organs do deteriorate as a dog or a cat ages. This is why we do a physical exam and recommend full blood work and a urinalysis before anesthesia and surgery. We routinely see older pets with normal kidney function, normal liver function, normal red blood cell counts, normal everything. If one or several values are abnormal, we need to know before anesthesia and surgery, because we may change a few things. For example, abnormally high kidney values may mean that a pet will be on IV fluids before anesthesia can be undertaken safely. We may also choose different anesthesia drugs and different pain killers after surgery if the bloodwork is worrisome. In other words, it may be much safer to anesthetize a healthy 12 year old patient with normal blood work than a sick 5 year old with kidney or liver disease. This is the difference between a pet’s actual age and the “functional” age, which takes into account all health factors and not only the age. Age (actual age) is merely a number. Health (functional age) is what we should focus on. Another common question I hear is "How old do (insert breed) get?" Books and web sites give us the answer to that tricky question. Yet those numbers are merely averages. It means that some pets live less, and some pets live longer. Just like in people, how long a pet will live is a guessing game at best. And sure enough, vets often see dogs and cats who beat the published averages.
Pets do live longer and longer, thanks to better vaccines, better drugs, better diets, better surgeries, better dental care... and above all more dedicated pet owners. After all, over the years, most pets progressively moved from the barn, to the back yard, to the mud room, to the living room, and now to the bedroom! Here is the bottom line: When the physical exam and blood work are fairly normal, the pet is in overall good health, and has a fixable problem, I tend to believe that this pet is a good candidate for anesthesia and surgery. If you have any questions or concerns, you should always visit or call your veterinarian – they are your best resource to ensure the health and well-being of your pets. Reviewed by: Rebekah Mack, DACVIM-SAIM Post by: Dr. Nancy Kay, DVM, DACVIM Dog Checkups & Preventive CareHas your Yorkshire terrier transitioned into his teens? Is the hair on your golden retriever’s muzzle now a lovely shade of gray? If so, it’s likely that some medical issues have accompanied your dog’s aging process. Examples include:
1. Learn as much as possible When a new medication is prescribed for your dog, talk with your veterinarian to gather answers to the following questions:
2. Read the label The prescription label often contains useful information intended to ensure that the medication works well. Read the label carefully to find instructions such as:
3. Get the help you need to achieve compliance Some dogs are real stinkers when it comes to sitting still for eye drops or swallowing a bitter tasting pill. Rely on your veterinary staff members to provide you with their tricks of the trade. Often, a simple suggestion can dramatically reduce the amount of “medication stress” for you and your dog. 4. Play by the rules It is in your dog’s best interest to give medications exactly as prescribed. If doing so isn’t feasible because of your schedule or simply doesn’t feel like the right thing to do, rather than skipping dosages or discontinuing treatment, have a frank discussion with your veterinarian. Almost always there will be other options to consider. 5. Refills Keep in mind that, in addition to authorizing refills for your dog’s medications, your veterinarian is juggling a whole host of other job responsibilities. For this reason, don’t wait until you are down to the last pill to request a refill. Provide at least two to three days notice. 6. Double check refills Accurately filling a prescription requires several steps:
7. Set up a system If you are giving multiple medications to your senior dog, it makes good sense to create a system that prevents missed doses or double dosing. Such goofs are easy to make, particularly when more than one person in the household is responsible for administering medications. Use of a chart that can be checked off when medications are given or a pill organizer (the plastic box with individual compartments) can cut down on dosing errors. 8. Online pharmacies Purchasing prescription drugs online comes with its pluses (cost and convenience) and minuses (potential for incorrect formulation, improper storage, dosage inconsistencies). If you are interested in purchasing your dog’s medications online, talk about this with your veterinarian and ask for a recommendation for a reputable company. 9. Air travel If you and your dog travel by plane, be sure to keep his medications with your personal belongings, in the cabin, rather than in the baggage compartment. Otherwise, a lost suitcase can translate into a huge hassle trying to refill medications on the fly. 10. Biannual exams
Any dog who has achieved the rank of “senior citizen” is well served by a veterinary exam at least twice a year. This is particularly true for dogs receiving medications. The office visit provides an opportunity to discuss how the drugs are working and how well they are being tolerated. Blood testing can gauge the effectiveness of some medications as well as screen for harmful side effects. Lastly, a significant change in your dog’s body weight may warrant a dosage change in his medication. If you have any questions or concerns, you should always visit or call your veterinarian -- they are your best resource to ensure the health and well-being of your pets. Posts by: Steve Dale, CABC Learn from Dr. Gail Golab, Chief Veterinary Officer at the American Veterinary Medical Association (AVMA) and the news from IDEXX Laboratories. IDEXX tested thousands of dogs and cats and saw no positive results. All Pet Health People continue to ask and I am repeating the info as not everyone sees everything posted. Dr. Gail Golab of the American Veterinary Medical Association in conjunction with the CDC answer your most common questions regarding pets and COVID-19
Veterinarians deal with corona viruses a lot and have for a very long time, canine and feline corona viruses – which the two species don’t share with one another or share with people. Also, when we get the common cold it’s usually a human corona virus (not to be confused with the novel corona virus which is now impacting the entire planet) and dogs and cats have never gotten colds from humans. But as Dr. Golab notes, this virus is different, and it’s novel; we’re still learning about it.
IDEXX Laboratories, Inc. announced that the company has tested thousands of dogs and cats for the SARS-CoV-2 virus (COVID-19), and thus-far not a single positive test. These new test results align with the current expert understanding that COVID-19 is primarily transmitted person-to-person, and is now considered a human corona virus. IDEXX press release: "IDEXX Laboratories, Inc. (NASDAQ: IDXX), a global leader in veterinary diagnostics and software, today announced that the company has seen no positive results in pets to date of SARS-CoV-2, the coronavirus strain responsible for the coronavirus disease 2019 (COVID-19) respiratory outbreak in humans. IDEXX evaluated thousands of canine and feline specimens during validation of a new veterinary test system for the COVID-19 virus. The specimens used for test development and validation were obtained from specimens submitted to IDEXX Reference Laboratories for PCR testing. These new test results align with the current expert understanding that COVID-19 is primarily transmitted person-to-person and supports the recommendation against testing pets for the COVID-19 virus. For dogs or cats presenting with respiratory signs, the recommendation is to contact a veterinarian to test for more common respiratory pathogens. “Should leading health authorities determine it is clinically relevant to test pets for the COVID-19 virus, IDEXX will be ready to make the IDEXX SARS-CoV-2 (COVID-19) RealPCR™ Test available,” said Jay Mazelsky, President and Chief Executive Officer of IDEXX Laboratories. “Pets are important members of our family, and we want to keep them healthy and safe. We will continue to monitor COVID-19 and pet health across our global IDEXX Reference Laboratories network as this situation evolves.” IDEXX Reference Laboratories is a global network of more than 80 laboratories united by a shared commitment to advancing pet care. IDEXX never stops looking for new ways to do more and discover more to enhance the health and well-being of pets, people, and livestock. Customers worldwide benefit from the company’s sophisticated network of veterinary reference laboratories in the United States, Canada, Australia, New Zealand, Japan, South Korea, South Africa, Brazil, and across Europe, which offer the most complete and advanced menu of tests in the industry." Still, Dr. Golab says use common sense regarding interactions with dogs and cats. It makes sense to wash hands after handling any animal. If you are a positive for COVID-19, it probably makes sense to have someone else in the home care for the animal (if possible). Dr. Golab agrees with that in this time of great stress, hearing cats purr in our ears and taking walks with our dogs can help us to feel warm and fuzzier.
COVID-19 Spread on Surfaces, such as Pets? Q: Can pets serve as fomites in the spread of COVID-19? A: Dr. Golab answers, “COVID-19 is usually primarily transmitted when there is contact with an infected person’s bodily secretions, such as saliva or mucus droplets in a cough or sneeze. COVID-19 might be able to be transmitted by touching a contaminated surface or object (i.e., a fomite) and then touching the mouth, nose, or possibly eyes, but this appears to be a secondary route. Smooth (non-porous) surfaces (e.g., countertops, door knobs) transmit viruses better than porous materials (e.g., paper money, pet fur), because porous, and especially fibrous, materials absorb and trap the pathogen (virus), making it harder to contract through simple touch. Because your pet’s hair is porous and also fibrous, it is very unlikely that you would contract COVID-19 by petting or playing with your pet. However, because animals can spread other diseases to people and people can also spread diseases to animals, it’s always a good idea to wash your hands before and after interacting with animals; ensure your pet is kept well-groomed; and regularly clean your pet’s food and water bowls, bedding material, and toys.” The American Veterinary Medical Association is the go-to resource regarding COVID-19 and pets. Reviewed on: Friday, March 20, 2020 Every day, Pet Poison Helpline receives dozens of phone calls from dog owners and cat owners saying “My cat ate a lily!” or “My dog ate a plant. Is it poisonous?” Some of the most poisonous plants for dogs and cats are reviewed below. While there are thousands of species of plants and flowers, only a small percentage of plants are truly dangerous and poisonous to your pet. Make sure you know which plants are most deadly to avoid your dog or cat from getting into these poisonous flowers and poisonous plants!
This is only a partial list of poisonous plants. For a more complete list of plants poisonous to cats and dogs, visit our Poison List.
If you suspect your pet has ingested any of these items or any other questionable substance, call Pet Poison Helpline at 855-764-7661 or your veterinarian for assistance. Accurate and timely identification of the suspected substance is very important. Having the container, package, or label in hand will save valuable time and may save the life of your pet. Post by: Dr. Nancy Kay, DVM, DACVIM Dog Toxins & PoisonsFor some folks, the start of a new year is a catalyst to lose weight and this may mean switching from plain old sugar to lower calorie sweeteners. Xylitol is one such sugar substitute that is safe for human consumption, but is toxic for dogs. In fact, it can be deadly.
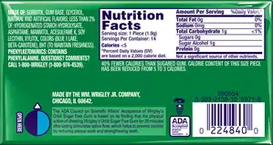
Additionally, compared to sugar, it causes very little insulin release in people and insulin is not required for it to be put to use as an energy source for the body. Lastly, xylitol has been shown to prevent mouth bacteria from producing acids that damage the surfaces of the teeth. For this reason, xylitol is commonly included in toothpastes, sugar-free gum, and other oral care products.
Xylitol Toxicity in dogs After a dog consumes a significant amount of xylitol, there is a massive release of insulin from the pancreas. This, in turn, results in a dangerously low blood sugar level and symptoms such as weakness, trembling, seizures, collapse, and even death. At higher dosages, xylitol can cause massive liver destruction (known as necrosis) in which large numbers of liver cells die abruptly. This produces an acute health crisis and, in many cases, death. Vomiting is often the first symptom of xylitol toxicity. Other symptoms related to the low blood sugar level develop within 30 minutes to 12 hours following consumption. When xylitol-induced liver damage occurs, blood liver enzyme values typically begin increasing within 12 to 24 hours. The dose of xylitol considered to be toxic for dogs is 0.1 gram or more of xylitol per kg of the dog’s body weight. What about cats and xylitol? While xylitol ingestion in cats does cause a drop in blood sugar, this rarely happens. This is because, unlike dogs, most kitties have very discriminating palates- they don’t choose to eat products containing xylitol.
The prognosis for xylitol toxicity varies and depends on how promptly the dog receives treatment as well as the amount of xylitol that was consumed.
Believe it or not, some products advertised specifically for dogs, such as toothpaste, contain small amounts of xylitol! What are these manufacturers thinking?!
Not all product labels clearly state if they contain xylitol. If a label states only, “artificially sweetened,” presume that it contains xylitol. If you opt to use xylitol-containing products in your household, be sure to keep them completely out of your clever dog’s reach. What to do if your dog eats xylitol If you believe that your dog has just eaten (as in you just watched it happen) something containing xylitol, contact a veterinary hospital staff member right away. You might be advised to induce your dog to vomit at home. This is accomplished by forcing your dog to swallow hydrogen peroxide. If you’re not really sure when the xylitol was consumed (you’ve just returned home from work and the remains of sugar-free gum wrappers are decorating the couch), transport your dog to a nearby veterinary clinic or 24-hour emergency hospital right away. Be sure to take the label of the consumed product with you. Time is always of the essence when treating xylitol toxicity. Look around your house and see if you have any xylitol-containing products. What did you find? If you have any questions or concerns, you should always visit or call your veterinarian -- they are your best resource to ensure the health and well-being of your pets. Resources
Reviewed by: Bill Saxon DVM, DACVIM, DACVECC Posts by:
Dr. Ernie Ward, DVM Dog Checkups & Preventive Care Dogs have 42 smile generators. Keeping those 42 teeth strong, healthy, and happy is essential to preventing illness, pain, and may extend longevity. Each February, U.S. veterinarians celebrate National Pet Dental Health Month to raise awareness about the dangers of oral diseases such as gingivitis, tooth abscesses, and mouth tumors. While I’ll be the first to admit it’s not a thrilling party theme, it is an incredibly important topic that directly affects every dog’s quality of life. To get this party started, I’d like to share five of my top tips for a healthier dog smile! 1. Daily brushing The foundation of a good oral care regimen for your dog is daily brushing. It can seem like a lot to brush your pet’s teeth daily, but it’s my professional obligation to remind you why it’s important. Daily brushing removes the biofilm and plaque created by mouth bacteria and helps avoid most oral diseases. That’s why we spend two to three minutes twice a day brushing our own pearly whites; we fear the dentist’s drill and the threat of root canals (well, at least I do). Once you train your pooch to sit still for a couple of minutes while you clean his teeth, you’ll discover how fast and easy it is. Here are my 7 simple steps to teaching your dog to tolerate the toothbrush:
No matter what, some pet parents simply can’t brush their dog’s teeth. If you fall into that category, think beyond the brush. Daily oral swishes and rinses, chew treats containing anti-plaque ingredients, and specialized teeth-cleaning diets are easy options. Be honest with your veterinarian if you struggle to clean your dog’s teeth; ask for alternatives to tooth brushing. I almost always find another technique the pet parent can use. Are these substitutes as good as brushing? Of course not. But they’re infinitely better than no oral care, and some work nearly as well. 3. Monthly mouth check In addition to daily oral care, mark your calendar for a monthly peek inside your pet’s mouth. Look for reddened or puffy gums, cracked or broken teeth, and unusual color changes, growths or swellings. Any bleeding, pus, or discharges from teeth and gums should be reported to your veterinarian immediately. While you’re checking the teeth, be sure to feel the throat for swollen lymph nodes, the eyes for cloudiness or changes in coloration, and the tummy for tenderness or masses. Identifying subtle changes early can help prevent significant diseases later. 4. Yearly vet check No discussion of oral health would be complete without mentioning the importance of annual veterinary checkups. Your veterinarian will carefully examine your pet’s oral cavity for any problems difficult to notice at home. Oral health may impact your dog’s entire body: infection in the mouth is reported to cause infection in the heart, kidneys, and elsewhere. A complete annual exam with basic bloodwork and complete urinalysis for adult dogs is what I recommend. The exam should be every 6 to 12 months for older canines as this can help with early disease diagnosis and optimize outcomes. 5. Veterinary dental cleaning There’s no substitute for regular dental cleanings by your veterinarian. Every one to three years, your pet will likely need to have his teeth professionally cleaned. In addition to producing a sparkling smile, the most important work occurs out of sight, beneath your dog’s gum line. Your veterinarian will carefully clean every tooth surface and remove plaque and tartar from hard-to-reach recesses below the gums and between teeth. Unchecked and uncleaned, pathogenic bacteria will eventually cause significant gum recession, resulting in oral pain and tooth loss. Tooth abscesses have been linked to heart valve infections and other serious medical conditions. The next time your veterinarian recommends a dental cleaning, remember the procedure is much more than cleaning teeth; it’s about preventing disease. There are many, many reasons to keep your dog’s smile healthy. Good health begins in the mouth. A healthy smile suggests a healthy pet. Try these five tips and ask your veterinarian for five more. Together we can help our pets live the longest, highest quality of life possible. Keep brushing and keep smiling! If you have any questions or concerns, you should always visit or call your veterinarian -- they are your best resource to ensure the health and well-being of your pets. Reviewed by: Dr. Celeste Clements, DVM, DACVIM Reviewed on: Tuesday, January 24, 2017
The minimal amount of time it takes for an attached tick to transmit disease is not known. The time it takes to transmit diseases is affected by the type of disease organism, the species of tick, etc. However, in general, if a tick is removed within 16 hours, the risk of disease transmission is considered to be very low. Therefore, owners can usually prevent disease transmission to their pets by following a regular schedule to look for and remove ticks.
Outdoor Environmental Control Treating the yard and outdoor kennel area with acaricides (tick pesticides) is an important tool in the arsenal against ticks. There are products that can be used to spray the outdoor area. However, you should not rely on spraying to reduce your risk of infection. If you have health concerns about applying acaricides, check with local health or agricultural officials about the best time to apply acaricides in your area, identify rules and regulations related to pesticide application on residential properties, and consider using a professional pesticide company to apply pesticides at your home. You can also create a tick-safe zone in your yard by using some simple landscaping techniques that can help reduce tick populations:
Indoor Environmental Control If ticks are indoors, flea and tick foggers, sprays, or powders can be used. Inside, ticks typically crawl (they don't jump) up and may be in cracks around windows and doors. A one-foot barrier of insecticide, where the carpeting and wall meet, can help with tick control. Prevent Ticks from Attaching
How To Remove A Tick With Tweezers
Risk of disease transmission to you, while removing ticks, is low but you should wear gloves if you wish to be perfectly safe. Do not apply hot matches, petroleum jelly, turpentine, nail polish, or just rubbing alcohol alone (the tick must be pulled out after application of alcohol) because these methods do not remove the ticks and they are not safe for your pet. Watch for Infection and Diseases After you pull a tick off, there will be a local area of inflammation that could look red, crusty, or scabby. The tick’s attachment causes irritation. The site can get infected; if the pet is scratching at it, it is more apt to get infected. A mild topical antibiotic, such as over-the-counter triple antibiotic ointment, can help but usually is not necessary. The inflammation should go down within a week. If it stays crusty and inflamed longer than a week, it might have become infected. Ticks can transmit diseases to pets and humans that the ticks contracted from a previous host. Although ticks can transmit diseases, ticks are usually nothing more than a nuisance. The best approach is to prevent them from embedding, and once embedded, to remove them quickly. As long as you stay on top of the situation, your pets should cruise right through the tick season with no problems. Date Published: 05/29/2006
Date Reviewed/Revised: 03/19/2018 URL: https://veterinarypartner.vin.com/doc/?id=4952474&pid=19239 Posts by: Dr. Ernie Ward, DVM Each New Year we’re inundated with lists of things to do, buy, and become. We read these lists, make promises to ourselves, and then promptly forget it ever happened by February. This year I’m taking the opposite approach: Here are the things you definitely don’t want to do, purchase or aspire to be more like. It’s time for my New Year’s Don’ts for your pets. 1. Don’t buy junk food treats. You know what I’m talking about. Those tiny calorie grenades are killing your pet. This year, feed fresh crunchy veggies or treats with simple ingredients such as sweet potatoes. 2. Don't ignore pet food labels. If you can’t comprehend what’s in your pet’s food, imagine how your pet must feel. The most important decision you make for your pets each day is what you feed. Choose wisely. Their health depends on it. 3. Don’t make excuses to skip walks. You both need to walk more. Buy a coat, umbrella or even a pair of galoshes, but don’t miss your daily walks. You’ll both live longer and be healthier because of it. [Watch What Happens When These Dogs Hear the Word “Walk”] 4. Don’t avoid the animal shelter. Go visit your local animal shelter so you can see for yourself what’s working and what needs to be fixed. I hear too many complaints about animal shelters from pet parents who’ve never set foot in one. How can we make something better when we don’t know what’s wrong? I know it’s painful and you want to take all the animals home with you, but you’ve got to do it. If you’re truly concerned about the state of stray animals in your hometown, go visit, talk to shelter employees and decide how you can help. [5 Ways to Help Your Local Shelter] 5. Don’t put off your pet’s exam. I know money’s tight but that little lump, cough or limp may be the start of something more serious. Often I’m left with simply too little time to help an ill patient. If I had a quarter for every case I could’ve saved had I only seen it six months earlier, I’d be retired by now, or at least have an enormous jar of quarters. Add to this, don’t go to the vet only when your pet is sick. My mission as a veterinarian is to preserve health and prevent illness. Going to the vet or physician should be an opportunity to learn how to stay healthier longer. You should leave each appointment with advice on how to improve your or your pet’s life. If not, ask for it. If you don’t get it, find it elsewhere. Life is for living, not recovering. Learn how to help you pet live an optimal life by working closely with your veterinarian on a regular basis. [My pet's perfectly healthy! Why should I see my veterinarian?] 6. Don’t forget your dog or cat’s heartworm preventive. Heartworm disease is fatal to dogs and cats. There is no treatment for cats and the medication used to treat dogs is costly, takes months to work, and carries potential health risks. Think your indoor cat isn’t at risk? Not according to research. Never gamble with your dog or cat’s heartworm protection. The stakes are too high and often end in death or serious damage. [What You Need To Know About Heartworm Disease] 7. Don’t ignore that pesky behavior. Little behavior problems turn into big troubles, quickly. If your dog is barking at passing cars, lunging on the leash, or jumping up on guests, talk to your vet (that’s our job). If you intervene with behavior problems early, you can often correct them easily. Wait until your dog is biting the delivery man, and it may take a while. 8. Don’t forget to hug your pet each day. And be thankful for all you have this year. Take time each day to reflect on one thing you have, that you’re grateful for. We are so fortunate to share our days with such wonderful, caring creatures. If you have any questions or concerns, you should always visit or call your veterinarian -- they are your best resource to ensure the health and well-being of your pets. The opinions and views expressed in this post are those of the author's and do not necessarily represent the beliefs, policies or positions of PetHealthNetwork.com, IDEXX Laboratories, Inc. or its affiliates and partner companies. Dr. Ernie Ward, DVM Ernie has more than 20 years of experience in the veterinary industry and is a well-known veterinarian, media personality and author. He is also a founding member of IDEXX’s Pet Health Network team. Read more > Reviewed by:
Graham Bilbrough, MA, VetMB, CertVA, MRCVS Reviewed on: Wednesday, December 6, 2017 © 2019 IDEXX Laboratories, Inc. All rights reserved. |
Archives
November 2023
Categories |
|
HELPFUL INFORMATION
Office Hours
Monday: 8AM – 6PM Tuesday: 8AM – 6PM Wednesday: 8AM – 8PM Thursday: 8AM – 8PM Friday: 8AM – 5PM Saturday: 8AM - 12PM Sunday: CLOSED |
LOCATION
AND DIRECTIONS Salem Veterinary Hospital
2159 Lynnhaven Parkway, Suite 105B Virginia Beach, VA 23456 |
CONNECT
WITH US! Phone (757) 427-2222
Fax (757) 467-5699 Email: salemvetvb@gmail.com |
Site powered by Weebly. Managed by IDEXX Laboratories

















































 RSS Feed
RSS Feed